What is Breast Thermography?
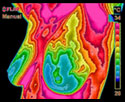
An infrared camera and computer system digital infrared imaging are used to measure heat from the surface of the breast to produce an image which can be evaluated for abnormalities. This modality has been in use since the 1960s and approved by the FDA in 1982 for use as an adjunctive breast cancer screening procedure. According to the American Cancer Society Breast Cancer Guidelines and Statistics you should have an initial infrared scan by age 20. Then a scan every 3 years between 20-30 years. At 30, you should have a scan every year.
The use of Digital Infrared Imaging (DII) is based on the principle that metabolic activity and vascular circulation in both pre-cancerous tissue and the area surrounding a developing breast cancer is almost always higher than in normal breast tissue. In an ever-increasing need for nutrients, cancerous tumors increase circulation to their cells by holding open existing blood vessels, opening dormant vessels, and creating new ones (neoangiogenesis). This process frequently results in an increase in regional surface temperatures of the breast. DII uses ultra-sensitive medical infrared cameras and sophisticated computers to detect, analyze, and produce high-resolution images of these temperature variations. Because of DII’s extreme sensitivity, these temperature variations may be among the earliest signs of breast cancer and/or a pre-cancerous state of the breast.
- Gautherie, Ph.D.; Thermobiological Assessment of Benign and Malignant Breast Diseases. Am. J. Obstet. Gynecol., 1983; V 147, No. 8: 861-869.
- Gamigami, M.D.; Atlas of Mammography: New Early Signs in Breast Cancer. Blackwell Science, 1996.
- Keyserlingk, M.D.; Time to Reassess the Value of Infrared Breast Imaging? Oncology News Int., 1997; V 6, No. 9.
- Ahlgren, M.D., E. Yu, M.D., J. Keyserlingk, M.D.; Is it Time to Reassess the Value of Infrared Breast Imaging? Primary Care & Cancer (NCI), 1998; V 18, No. 2.
- Belliveau, M.D., J. Keyserlingk, M.D. et al ; Infrared Imaging of the Breast: Initial Reappraisal Using High-Resolution Digital Technology in 100 Successive Cases of Stage I and II Breast Cancer. Breast Journal, 1998; V 4, No. 4